The nasal drug delivery landscape has evolved tremendously since its inception several decades ago. In its early years, nasal delivery was largely confined to the administration of locally acting treatments for decongestion and rhinitis. Some of the earliest nasal sprays date back to the 1950s and 1960s, when two over-the-counter (OTC) decongestants became available for widespread use. But, in fact, if we look back even further, nasal delivery of drugs dates back to ancient civilisations. Nasaya Karma is a recognised form of treatment in the Ayurvedic system of Indian medicine. More recently, pharmaceutical drug developers have begun to research nasal delivery as an alternative to common routes of administration (RoA), such as oral and parenteral. In part, this is due to the high permeability of the nasal epithelium, allowing a higher molecular mass cut-off at approximately 1000 Da, as well as the rapid drug absorption rate with plasma drug profiles, which are sometimes almost identical to those of intravenous injections.
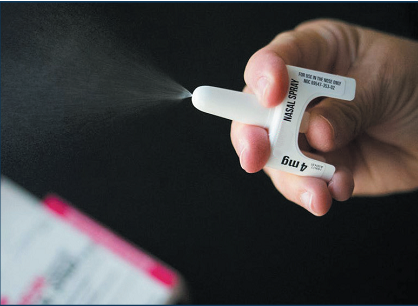
Intranasal drug delivery for systemic application is now an option for several more indications – most notably for rescue therapies because of its rapid onset of action, but also for infectious disease prevention, pain, central nervous system conditions and a variety of others. We have witnessed several first-of-a-kind nasally delivered treatments, such as: Narcan® (naloxone) for opioid overdose from Emergent BioSolutions (MD, US); an antidepressant, Spravato® (esketamine), from Janssen (J&J); a nasal diazepam for seizures, marketed as Valtoco® by Neurelis (CA, US); and, from Oyster Point Pharma (NJ, US), Tyrvaya® (vareniciline) for dry eye disease. The rate at which intranasally delivered molecules have been approved has also increased drastically over the past five years. Now, clinical research is underway to evaluate intranasal delivery as a means of delivering drugs to the brain across the blood-brain barrier, with therapies for Alzheimer’s disease and other degenerative brain diseases in active development.
REGULATORY PERSPECTIVE
While the number of drugs being delivered intranasally has grown in recent years, and the acceptance of these products has advanced greatly, the requirements necessary to gain regulatory approval are still evolving. The latest approved guidance for these products was issued in July 2002. This guidance, along with the requirements listed in the US Pharmacopeia, are the key points of reference for sponsors seeking to gain approval for their products. However, the chemistry, manufacturing and controls provided for nasal spray drug products in the guidance document lack direction for specific unit dose delivery systems, intranasal powder delivery, controls for vaccines, and biotherapeutic modalities. As regulatory bodies look to address these new modalities, product manufacturers have needed to interpret requirements by extrapolating guidance directed at other forms of orally inhaled and nasal drug products, while still following product-specific guidances as they relate to their programme.
FORMULATION STRATEGIES
 Bioavailability, solubility and viscosity are critical aspects of the formulation that must be assessed during nasal spray development. Physical barriers are also a concern, as the complex geometry of the nasal passages makes reliable and efficient delivery to the mucosal surfaces deep in the nasal cavity a challenge. Lastly, nasal clearance should be considered. The epithelium of the nasal passage is covered by a mucus layer that entraps particles and is cleared from the nasal cavity by the action of the nasal cilia, which renew the mucus every 10–15 minutes by moving it through the nose at an approximate rate of 5–6 mm/min. Drugs with poor solubility would be particularly challenged by mucociliary clearance, as they must guarantee sufficient bioavailability to achieve the desired therapeutic effect.
Bioavailability, solubility and viscosity are critical aspects of the formulation that must be assessed during nasal spray development. Physical barriers are also a concern, as the complex geometry of the nasal passages makes reliable and efficient delivery to the mucosal surfaces deep in the nasal cavity a challenge. Lastly, nasal clearance should be considered. The epithelium of the nasal passage is covered by a mucus layer that entraps particles and is cleared from the nasal cavity by the action of the nasal cilia, which renew the mucus every 10–15 minutes by moving it through the nose at an approximate rate of 5–6 mm/min. Drugs with poor solubility would be particularly challenged by mucociliary clearance, as they must guarantee sufficient bioavailability to achieve the desired therapeutic effect.
One approach to increasing nasal residence time is through the use of muco-adhesive systems, which retain the drug solution longer in the nose. Another is the use of permeation-enhancing technologies, which facilitate both the rate and extent of absorption. The development and use of permeation enhancers significantly improves the absorption of high molecular weight drugs as well. These permeation enhancers can facilitate the absorption of molecules up to 40 kDa, enabling the nasal delivery of peptides and proteins that would have traditionally had to be delivered via the parental RoA to avoid enzymatic degradation in the gastrointestinal tract.
CURRENT NASAL SPRAY DEVICE LANDSCAPE
The bulk of the nasal drug delivery landscape uses three types of device: unit-dose, bi-dose and multidose; with unit- and bi-dose being used for acute/rescue indications, and multidose for chronic indications.
The allergic rhinitis market generally uses multidose nasal pumps, primed by the user and capable of delivering formulations with volumes from 25–140 μL. These devices can dose several varieties of formulations, such as solutions and suspensions for chronic indications. On the other hand, unit- and bi-dose devices are portable and can therefore easily be carried about one’s person. They can be actuated easily during a crisis, and they accurately deliver necessary drug volumes at any orientation, without requiring the pump to be primed.
Factoring in the long history of nasal OTC products and their wide availability, patients have become increasingly familiar with this RoA. Ultimately, this decreases the required learning curve for new intranasal therapies in the unit- and bi-dose configurations. That said, additional verbal and written patient education is required to help ensure correct and compliant dosing.
As noted prior, the nasal market has grown significantly over the last several decades, from a market comprised of largely OTC multidose delivery to diversified offerings using specialised unit- and bi-dose devices. This evolution has also led to several advancements within nasal device technology to improve reliability over the years. These advancements, along with addressing challenges surrounding formulations to be delivered through the nasal cavity, can promote positive results.
Another reason for the growth in the unit and bi-dose segment of nasal drug delivery is the covid-19 pandemic, which fuelled vaccine development. There are over 100 vaccines or prophylactic treatments for covid-19 currently in late-stage clinical trials, some of which are being developed for intranasal administration, which aim to improve mucosal immunity efficacy and allow for faster, easier and patient-friendly global immunisation.6 Even as covid-19 case rates decline in number and the enthusiasm to fund some of these programmes starts to wane, the pandemic’s legacy includes an advancement in the knowledge and clinical research of nasal delivery of biotherapeutics for infection prevention, and some promising product candidates remain in development. Just recently, the regulatory bodies within China, India, Iran and Russia have approved the use of four intranasal covid-19 vaccines.
We now have several game-changing products, spanning a vast number of therapies, entering the space that will certainly advance the industry even further. There are currently more than 150 molecules at various stages of development within the nasal pipeline, with projections indicating the number will grow to over 195 by 2027. The development pipeline remains healthy and robust with both substantial investment in preclinical molecules and consistent maturation of programmes in the existing pipeline. The sizeable portfolio of preclinical molecules should lead to a number of commercial opportunities.
Overall, the nasal delivery market is expected to experience approximately 6% compound annual growth rates over the next decade. This would drive the already significant market value of the global nasal drug delivery market from US$45 billion (£40 billion) in 2019 to an estimated $88 billion by 2030. The covid-19 pandemic aside, the growth in nasal programmes can be attributed to new disease areas and modalities using this RoA (e.g. Parkinson’s disease, Alzheimer’s disease, anxiety and depression), as well as increased awareness, acceptance and the benefits and ease of self-administration of nasal therapies.
 In some instances, nasal delivery offers advantages over the most commonly used oral and injectable RoA, and over some less used, such as rectal administration. Unlike the oral and rectal RoA, nasal sprays avoid the biotransformation of the drug in the gut lumen prior to absorption and in the intestinal epithelium and/or liver after permeation of the intestinal mucosa but before entering systemic circulation, known as first-pass elimination. Nasal delivery also provides local protection at the nasal mucosa that could potentially assist at the point of entry to defend against viruses and bacteria – an added benefit.
In some instances, nasal delivery offers advantages over the most commonly used oral and injectable RoA, and over some less used, such as rectal administration. Unlike the oral and rectal RoA, nasal sprays avoid the biotransformation of the drug in the gut lumen prior to absorption and in the intestinal epithelium and/or liver after permeation of the intestinal mucosa but before entering systemic circulation, known as first-pass elimination. Nasal delivery also provides local protection at the nasal mucosa that could potentially assist at the point of entry to defend against viruses and bacteria – an added benefit.
CONCLUSIONS
Nasal devices have proven themselves to be incredibly reliable, providing accurate dosing whether administered by the patient themselves, by a caregiver or by emergency personnel. When replacing the injectable RoA, nasal sprays or powders obviate the need for needles, bypassing injection-related phobias and, in most cases, the need for healthcare practitioner support.
It is essential that both the formulation and device are compatible if they are to support successful intranasal drug delivery. Formulation improvements, the potential use of permeation enhancers and new device technologies have led to the expansion of overall possibilities for device/formulation variations to create a successful final product with the optimal spray characteristics. Though complex, the nasal route is therefore an attractive alternative that provides access to highly vascularised mucosa, is easy to reach through self-administration and can, with the appropriate formulation and delivery system, deliver the drug dose conveniently and reproducibly while bypassing hepatic metabolism.
According to the materials:
https://ondrugdelivery.com/nasal-delivery-a-galaxy-not-so-far-away-a-brief-market-history-of-the-nasal-delivery-landscape/


